Are you really TAP-ing it right?
- Dr Arul James, MD, FRCA, FFPMRCA
- 10 hours ago
- 3 min read
What a major 2026 BJA review means for everyday regional anaesthesia practice
Zako J, Kevorkov A, Jeffries SD, Ramirez-Garcia Luna JL, Daccache N, Song K, Harutyunyan R, Ritchie C, Cafferty O, Laferriere-Langlois P, Hemmerling TM.
Transversus abdominis plane block for postoperative pain management and opioid sparing: a systematic review and meta-analysis of randomised controlled trials.
British Journal of Anaesthesia. 2026;136(1):266–282. doi:10.1016/j.bja.2025.10.033
The above BJA systematic review and meta-analysis synthesised evidence from 123 randomised controlled trials evaluating transversus abdominis plane (TAP) blocks across a wide range of abdominal surgeries. The key message for practice is that TAP blocks have robust evidence for improving early postoperative analgesia within multimodal pathways, but their comparative performance against neuraxial techniques is context-dependent and not uniformly superior.
What the evidence supports
• Compared with placebo, TAP blocks reduced postoperative pain at 6, 12, and 24 hours, and reduced 24-hour morphine consumption, with substantial variability between trials.
• Compared with local wound infiltration, TAP blocks also reduced pain at 6, 12, and 24 hours and reduced 24-hour morphine consumption, again with marked between-study heterogeneity.
• Compared with epidural analgesia, TAP blocks showed a pain reduction at 12 hours, but no clear difference at 6 or 24 hours; evidence was limited and of low certainty.
• Compared with intrathecal morphine, TAP blocks showed no significant differences in pain scores or 24-hour morphine consumption within the included trials; certainty was generally low/very low.
Practical interpretation
• TAP blocks are best framed as multimodal, neuraxial-sparing analgesic options, particularly useful where neuraxial techniques are undesirable, impractical, or contraindicated.
• The literature shows high heterogeneity, and differences in technique and delivery can contribute to variable outcomes—supporting a training focus on sono-anatomy, probe control, needle alignment, and injectate-plane confirmation rather than memorising named variants.
From evidence to execution:
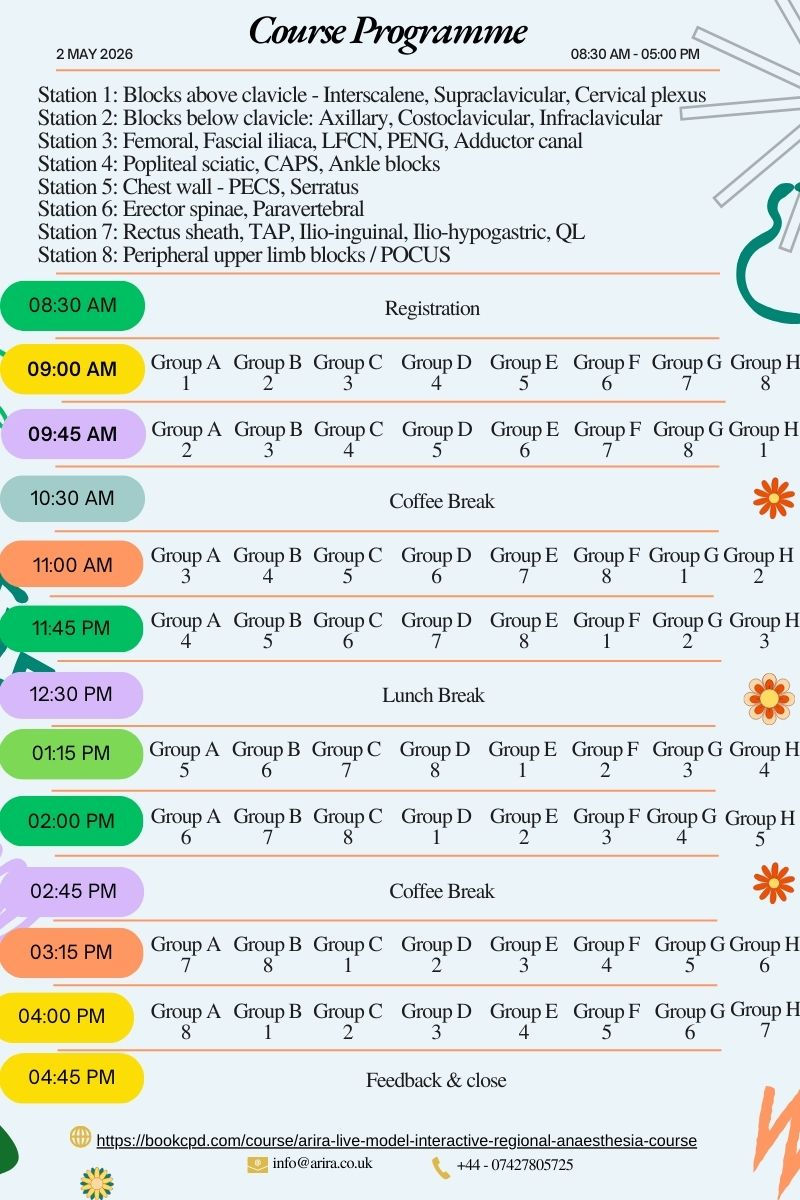
ARiRA Live – Model Interactive & Hands-On Course: 1–2 May 2026

Submit your abstracts for poster presentation now!
Two-Day Ultrasound-Guided Regional Anaesthesia Course
Designed from candidate feedback to maximise expert-led teaching & hands-on learning.
Day 1 – Friday 1 May 2026 | Online, Interactive
Live, faculty-led teaching focused on clear, applied anatomy
High-definition cadaveric dissections integrated with ultrasound correlation
Augmented reality and simulation-based videos to reinforce probe handling and spatial understanding
Structured, exam-focused teaching with EDRA Part 1 & 2 preparation tips
Interactive Q&A throughout to address common pitfalls and misconceptions
Optimised pacing to allow consolidation without cognitive overload
Poster presentation by candidates which will be published in ARiRA - Newsletter

Day 2 – Saturday 2 May 2026 | In-Person, Hands-On
Small-group live scanning on models to maximise probe time
Emphasis on sono-anatomy recognition, ergonomics, and image optimisation
Unhurried needling practice using dedicated needling phantoms
Protected time for repetition and self-directed practice, guided by expert faculty
Continuous faculty feedback tailored to individual experience level
Lunch and refreshments provided
What makes this course different
Designed around what previous candidates asked for: more scanning time, slower pace, clearer anatomy, and practical relevance
Faculty with extensive clinical & teaching experience
Balance of why and how, not just what—moving beyond atlas-style teaching
Focus on confidence, pattern recognition, and transferable scanning skills
Included with your course
1 year of complimentary ARiRA access
Full access to arira.co.uk, including:
Cadaver-based anatomy modules
3D and augmented-reality anatomy visualisation
Sono-anatomy libraries
Probe movement and image-formation concepts
Simulation-based learning to support ongoing practice
Who should attend
Anaesthetists preparing for EDRA examinations
Clinicians looking to consolidate or refresh core regional anaesthesia skills
Those seeking structured, high-yield teaching with genuine hands-on time
Registration
• Applying for RCoA CPD and ESRA DRA points
• Limited places to preserve hands-on quality



